BAMAKO, Mali—I was talking to Yaya Sarro, a molecular biologist at the National Laboratory, when the biological samples from the newest possible Ebola case arrived for diagnosis. It was six days after Mali’s first patient, a two-year old girl who had taken a long bus ride from Guinea with her grandmother and sister, tested positive for Ebola. She died on Oct. 24, 600 km northwest of the capital in Kayes. Now Malians, hospital staff, contact tracers, the ministry of health, a few journalists and a coalition of international partners were anxiously waiting for the next case to appear. Eighty-five people were under surveillance, mostly in Kayes, but some in the capital. Families were in isolation.
Two stocky doctors had brought the sample from Selingué, a town on the border between Guinea and Mali, where a man had died after presenting a few of the unspecific symptoms of Ebola’s profile. Hours earlier, the doctors took samples of his blood, saliva, and mucus from his nose. They packaged the samples in a plastic tube, triple-wrapped it in a custom box and drove to Bamako. They handed over the box as Yaya left to suit up.
Bamako’s national laboratory sits atop one of two wide hills behind the capital of Mali. On one peak is the presidential palace; on the other is the hospital and medical school. Inside is a level-3 biosafety laboratory (BSL), outfitted by the American National Institute of Health to handle Tuberculosis, HIV and as of this summer, Ebola. The lab is run by Malian doctors and infectious disease scientists. No one knows if or how the disease will spread in Mali; however it does, a drop of it will come to this lab first.
If Ebola stays in Mali, this lab will be the country’s invaluable resource. Amadou Kone, another molecular biologist, said that when the little girl’s samples arrived last week, they had results within hours. That is staggeringly fast and not just for West Africa. In April, before samples were tested here, a few cases of Ebola were suspected in Bamako. People were put into isolation, their samples sent to Dakar or Atlanta. The results took three weeks to come back while panic and rumor spread on the streets of the capital and frightened patients sat in quarantine. “Our work can allow families to go home,” Yaya said.
As Yaya and his colleague re-emerge in blue jumpsuits and step into the clean room’s antechamber, Dr. Ousmane Koita, who runs the lab, plays valet. We watched through glass windows.

Level-3 biosafety facilities have negative air pressure. They have backup systems and alarms should a ventilator malfunction. Their humidity and temperature are controlled. Air goes in but it does not go out. There is an autoclave, work hoods, boxes of gloves, paper towels, and bottles of disinfectant. Sound doesn’t move between the interior and the exterior. Ebola is designated a level-4 biosafety virus in Europe, America, Singapore and Australia: handling it requires showers, dressing procedures and total isolation from the rest of the building. But no level-4 facilities exist in West Africa—the nearest is in Gabon. So in April, when the disease was proving its tenacity in neighboring Guinea, American doctors saw the threat and nominated Bamako’s level-3 lab capable of diagnosing Ebola. That is how a room designed to protect researchers from TB and HIV became a room where they could also defuse the world’s scariest bug.




The white cardboard box of samples is sitting on the floor in the antechamber at Yaya and his colleague’s feet. They pull on Tyvek paint suits, grey booties, white respirator masks, plastic goggles. They look ready for a day of asbestos scrubbing. The purple, long-fingered gloves come on. Sarro tells me these are strong and expensive. Koita takes a roll of masking tape and winds it around Kone’s wrists. A second pair of gloves, a blue shower cap to cover the hair and the hood are pulled tight. Kone and his colleague are heating up; their hands look a little bit limper. They let Koita pull white bibs over their chests and tie them around the back. “Like a cook,” Sarro tells me. Finally, the plastic facemask. Koita turns them around and checks the points of vulnerability. He touches their wrists, their waist, their face; the valet checking his man before the duel against the box. Koita leaves the room. Yaya’s colleague opens the door to the lab, kicks the cardboard box through and seals himself in.


Within 15 minutes of opening the box, Yaya and his colleague have mixed the samples with lysing agents that destroy cellular structure, leaving behind a soup of impotent genetic material. They give us thumbs up. After marking the tubes with a Sharpie, they begin cleaning up and stripping down. Everything is slathered with disinfectant.
This part, crucial in any contact with possible Ebola, is geometrically confusing. They scrub everything down and squirt chlorine over their hands and clothes, then peel off their protective layers. First the facemasks, then the hoods, the goggles, and the top gloves all are flung into red biohazard bags. Soon their faces are exposed. They unzip their jumpsuits and shimmy, pulling the suits down and off with the gloves. But they’re still inside the dirty chamber, the level-3 biosafety containment lab, the place where a moment ago possible Ebola was assumed to be everywhere. They must pay attention, Sarro tells me, to pull from the inside of the suit only. That maintains the clean envelope they are creating. The gloved hands remove every piece, then come off themselves, from the inside, fingers last.

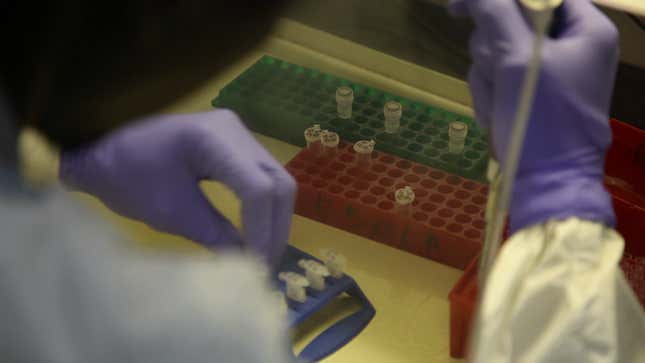

Within the hour the samples are under a new hood in the next room (biosafety Level-2, suitable for most biological and chemical agents), sitting in a red tray marked EBOLA along the side. The samples are in six small, milliliter doses, mixed with reagents and amplifying solutions. These are placed in an American-made Polymerase Chain Reaction machine, the workhorse of genetic analysis, which will alternate hot and cold over the next hour while enzymes make millions of copies of the suspect RNA. The results will be compared to the Zaire strain, the Uganda strain, the Sudan strain, and a control. A single genetic match, about 70 bases long, proves Ebola. It is 8pm. By 9:30pm, a green line on a computer screen will be flat if the dead man was negative, or curved gently upwards if he was positive.
For Sarro and Kone, diagnosing Ebola is no more frightening than diagnosing anything else. They joked in the BSL2 room that Ebola is a delicate bug, easy to break. Tuberculosis, which is airborne, is far scarier. For a molecular biologist, “at our level, the virus is always dead,” said Kone. Are they surprised to have identified Ebola in Mali? “No, it was a matter of time” said Dr. Koita. They are confident that if the government and health ministries track contacts and push public hygiene, Ebola will not last. Some responders are less sure. We eat bananas and soda in the break room after pumping hand sanitizer.
I knock on Koita’s door at 8:45pm—I want to know the shape of the green line. “The results,” he tells me, “go from here directly to the ministry and to the president.” Apparently information stays on the inside, and I’m outside.
Mali’s first Ebola case triggered a huge and swift response, motivating flights of experts from abroad and trucks of material to the affected site within days, in large part because this lab provided a diagnosis in real-time. I’m told the next day that Tuesday night’s sample was negative, as the doctors had expected. The body was released to the family
The biologists worked on Tabaski, the most important holiday for Malian Muslims. They work nights and weekends. They will likely be on-call for a long time.
